Osteoporosis is a condition in which the bones become weaker, making breakages more common. In this blog, we’re looking into how we can reduce the risk of osteoporosis.
What is Osteoporosis?
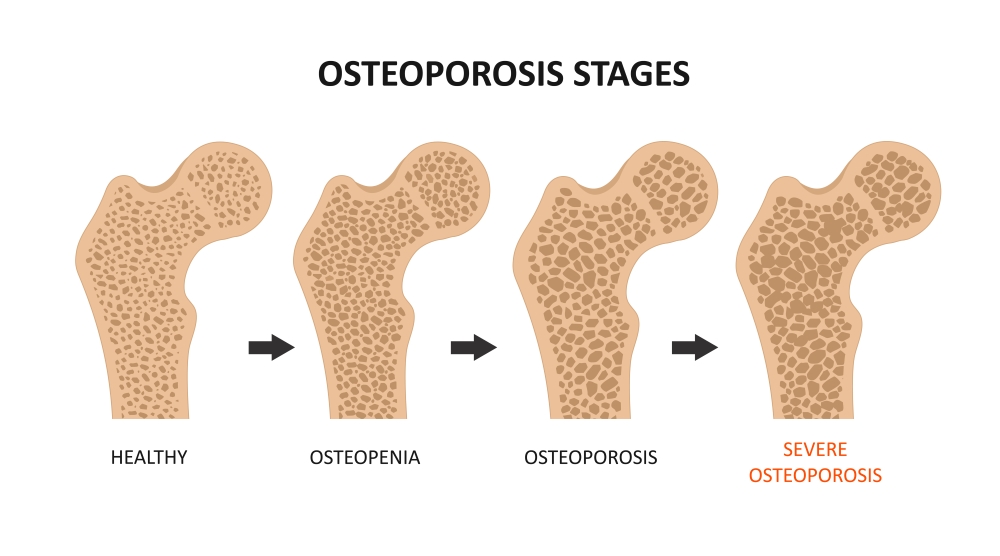
The internal structure of our bones resembles a honeycomb. As we age, this structure becomes less dense, with enlarged gaps, increasing the risk of fractures from seemingly minor injuries.
Throughout my career, I’ve observed elderly patients sustaining rib or spinal fractures from simple actions like coughing. This vulnerability is notably pronounced in women who experience a decline in bone mass, losing approximately 1-2% annually after menopause. Consequently, women tend to experience height loss and are at a higher risk of hip fractures, which are linked to elevated rates of severe illness and mortality.
How can we check our bone density?
FRAX assessment, employed by doctors, estimates fracture risk and guides further investigation. However, it’s crucial to note that FRAX isn’t definitive and acts as a guide, lacking consideration of all osteoporosis risk factors. For instance, a parent with osteoporosis who never suffered a hip fracture may not influence your assessed risk.
Calculate the ten-year probability of fracture with BMD here.
A bone density or DEXA scan is the most valuable test for assessing bone health. This painless and straightforward procedure involves lying fully clothed on an x-ray bed while images are captured.
Surprisingly, research indicates that only 20% of individuals who should undergo a DEXA scan are actually referred for one. Summerhill Health can facilitate private DEXA scans in Altrincham upon request.
Who should have a DEXA scan?
- All women 65 years of age and older
- All men aged 70 years and older
Women under age 65 with an additional risk for osteoporosis.
1. Women discontinuing oestrogen HRT or oestrogen deficiency (peri-menopausal and post-menopausal women)
2. Early or premature menopause (before age 45 years old)
3. History of amenorrhoea (no periods) for more than one year under the age of 42 years
4. History of maternal hip fracture that occurred after the age of 50 years
Men and women with other risk factors:
5. Eating disorders (current/past)
6. Men younger than 70 with testosterone deficiency
7. Adults of any age with fragility fractures – low impact fractures such as a wrist (colles) fracture
8. Men or women receiving or expected to receive steroid treatment for more than three months (e.g. >5mg Prednisolone for more than three months in a year)
Individuals beginning or receiving long-term therapy with a medication known to affect bone mineral density adversely:
- Anti-coagulants – warfarin, heparin
- Anti-epileptics
- Aromatase inhibitors, etc. (many other medicines that may cause osteoporosis)
Individuals of any age with x-ray evidence of:
- Low bone mass (osteopenia),
- Vertebral deformity (kyphosis)
- Presence of vertebral compression fractures.
Men and women of any age with a disease associated with a defect in bone development, low bone mass or bone loss, such as:
- Osteogenesis imperfecta
- Hyperthyroidism (overactive thyroid gland)
- Inflammatory bowel disease (IBD)
- Rheumatoid arthritis
- Growth hormone deficiency
Men and women of any age who have the following risk factors;
- Loss of height of more than 2cm
- BMI below 18
- Poor or mal-nutrition
- Excessive alcohol intake (>14 units a week)
- Current or ex-smokers
- Excessive exercise, particularly with inadequate calorie intake.
Medications that may cause osteoporosis
- Chemotherapy
- Radiation
- Levothyroxine
- Anticonvulsant therapy or anti-epileptic medications (phenytoin and phenobarbitone)- interfere with calcium absorption and production of Vitamin D
- Long-term heparin, Warfarin or lithium therapy
- GnRH analogues such as Zoladex
- LHRH analogues; testosterone suppression
- Prolactin-raising drugs such as antipsychotic medications, e.g. some SSRI and aromatase inhibitors for the treatment of Prostatic and Breast.
- Cancers e.g. Arimidex
- Diuretics such as Burinex and Lasix (furosemide)
- Proton Pump Inhibitors – omeprazole, lansoprazole
What can we do to reduce the risks of osteoporosis?
Educate young women
To reduce the risks of osteoporosis, we must empower young girls by educating them on the importance of maintaining a healthy weight and regular exercise. Both high and low Body Mass Index (BMI) values pose risks, as does crash dieting. Adequate calcium intake through diet plays a pivotal role in supporting bone health. Dietary calcium is notably superior to supplements in promoting bone health. Assess your calcium intake with the following link to ensure adequate consumption:
CALCIUM – Calcium Calculator | International Osteoporosis Foundation
Consider vitamin supplements
Consider a daily vitamin D supplement of 400-800 IU, particularly during winter or for women with limited sun exposure. Aim for 30 minutes of sun exposure twice a week to the arms, legs, and face without sunscreen to achieve adequate vitamin D levels.
Regular weight-bearing and strength exercises are essential to promote strong bones and muscular support for the skeleton.
Hormone Replacement Therapy – HRT
Certain medications, such as Hormone Replacement Therapy (HRT), can aid in preventing osteoporosis during its use and even for a period after cessation. However, current recommendations advise against using HRT solely for this purpose, except for younger menopausal women.
We can support you with all aspects of women’s health. Take a look at our wide range of services. Don’t hesitate to contact us if you have any questions regarding bone health and menopause – we’re more than happy to help. We hope this blog has been useful on how to reduce the risk of osteoporosis.
Dr Summerhill is a GP and Menopause Specialist. She qualified from Guy’s, King’s and St Thomas’s (GKT) School of Medical Education in London in 2007. She qualified as a GP from the Royal College of General Practitioners (RCGP) in 2015 and has undertaken specialist training in women’s health having achieved diplomas from the Royal College of Obstetricians and Gynaecologists (DRCOG) as well as the Faculty of Sexual and Reproductive Health (DFSRH). She has the Letter of Competence from the FSRH for both coils and implants. Dr Summerhill has undertaken extensive training in menopause management and holds an Advanced Menopause Specialist certificate with the Faculty of Sexual and Reproductive Healthcare.